Pain, Tight Tendons and Loose Ligaments
written for Pain Treatment Directory
Hello dear patients and friends. As a doctor of Musculoskeletal Medicine, it is one of my goals in life to get people out of pain! And I love to teach both patients and doctors about what is really going on with the pain in our bodies. With that aim in mind, let’s begin by understanding the true source of most pain that is not addressed by traditional medicine. This often includes the vague, frustrating diagnosis of Fibromyalgia.
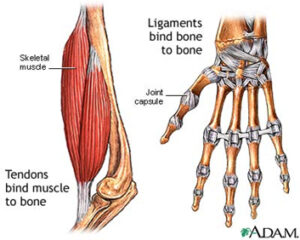 To get started we need to know some anatomy:
To get started we need to know some anatomy:
Ligaments: Hold bone to bone.
Tendons: Hold muscles to bones
Joints: Space between 2 bones, allowing motion of the bones.
The source of the pain around the bones and muscles is actually that the tendons are too tight, or the ligaments are too loose or both.
How do ligaments become too loose? Ligaments are fibers (made up of Elastin and Collagen) which have a certain amount of stretch and a certain amount of tightness. In every joint, the ligaments hold the joint in place allowing it to move the bones in the proper direction. We know abnormal movement in the joint is a very common source of arthritis. So the ligaments keep the joints from moving too much. In the knee joint, for instance, along each side is a ligament preventing the knee from going inward or outward when we walk.
Ligaments become too loose by:
1) Aging and Overuse: By far the most common. The ligaments start out as supple fibers and with the drying process (that accompanies aging and overuse) become similar to a frayed rope. As a result, they don’t hold the bones together as well.
2) Injury: Think of skiing where every leg is for itself and the lower leg is going sideways on the upper leg. This can stretch the side ligaments and sometimes result in small tears (degeneration) that don’t heal, leaving a person with a chronically unstable joint.
3) Genetics: Hypermobility: Some people have a different sort of collagen which results in too much motion in the ligament. This is not uncommon and is extremely underdiagnosed. Interestingly, being able to bend excessively it may be just a fun party trick until there is an injury and then the total body hypermobility announces itself. In this situation, people are unable to strengthen because their bones move out of place (which they are often unaware) and it hurts! When it is very significant it is called Ehlers- Danlos Syndrome.
4) Infection/ Certain Drugs: Rarely, an infection or certain drugs can cause weakness in the ligaments and tendons.
Why are Loose Ligaments painful? Because the bones will move too much. Many times, most people don’t even realize what is happening.
Then what happens? The body is amazing! It will compensate by tightening the tendons, in an attempt to keep us straight. Over time, with the tendons constantly contracted, the muscles become weak and painful in the region of the insertion into the bone, because they are always holding tight. So often times we have pain and tight “muscles” in a place that is not the source of the problem, and this can be very confusing.
How do we strengthen ligaments? The only way to strengthen ligaments is through PRP or dextrose prolotherapy. By making very precise injections of these safe substances directly into the problem ligament, we can strengthen them and return the patient to pain-free activity. This treatment promotes the body to heal those specific areas by its own natural process.
Tight Tendons:
We have discussed one source of tightness which is chronic contraction to counteract the loose ligaments. The other source of tightness is overloading the muscles. We all know what it feels like to have sore muscles after a heavy work out. This is not what I am referring to. This is, day after day, overusing the muscles so the tendons which hold the muscles begin to take the brunt of the problem and become chronically sore. So the pain will not be in the muscles, but at the attachment of the muscles next to the bones.
Wrong approach: Trying to strengthen the muscles. This won’t work because they are already on overload. This can be very frustrating because now the muscles are getting weak.
Better approach: Rest the muscles. This actually works, along with gentle strengthening as the tendon relaxes. However, this can take a very long time and as a result, the muscle gets even weaker and so the rehabilitation is very slow.
Best approach: Treat the tendon with Prolotherapy/PRP followed by gentle strengthening. This stimulates the body to heal the tendons naturally.
Worst approach: Treating the tendon with steroids which weakens and degenerates the tendon.
Do you or someone you know have mysterious pain, or “fibromyalgia”? This is frequently treatable with PRP or Dextrose Prolotherapy in the right hands. Stay tuned. In my upcoming blogs, we will address these pain syndromes, and the sane, effective path to healing. I hope you will come with me on this journey.
PS-using serious sterile precautions, we are open for consultations and treatment.
References:
1) Brian Halpern, Salma Chaudhury, Scott A. Rodeo, Catherine Hayter, Eric Bogner, Hollis G. Potter, Joseph Nguyen. Clinical and MRI Outcomes After Platelet-Rich Plasma Treatment for Knee Osteoarthritis. Clinical Journal of Sport Medicine, 2012; 1 DOI: 10.1097/JSM.0b013e31827c3846
2) Chang KV, Hung CY, Aliwarga F, Wang TG, Han DS, Chen WS.Comparative Effectiveness of Platelet-Rich Plasma Injections for Treating Knee Joint Cartilage Degenerative Pathology: A Systematic Review and Meta-Analysis.Archives of Phys. Med. Rehabil, 2014 March;95(3);562-575.doi; 10.1016/j.apmr.2013.11.006. Epub 2013 Nov 27
3) Cusi M; Saunders J; Hungerford B; Wisbey-Roth T; Lucas P; Wilson S. The use of prolotherapy in the sacroiliac joint. Br J Sports Med 2010;44: 100-104.
4) Freeman JW, Empson YM, Ekwueme EC, Paynter DM, Brolinson PG. Effect of Prolotherapy on Cellular Proliferation and Collagen Deposition in MC3T3-E1 and Patellar Tendon Fibroblast Populations. Transl Res. 2011 Sep;158(3):132-9.doi: 10.1016/j.trsl.2011.02.008. Epub 2011 Mar 21.
5) Gosens T, Peerbooms JC, van Laar W, den Oudsten BL. Ongoing Positive Effect of Platelet-Rich Plasma Versus Corticosteroid Injection in Lateral Epicondylitis: A Double-Blind Randomized Controlled Trial With 2-year Follow-up [In Process Citation] Am J Sports Med (United States), Jun 2011, 39(6) p1200-8.
6) Hackett GS, Hemwall GA, Montgomery GA : Ligament and Tendon Relaxation treated by Prolotherapy Charles C Thomas Publisher
7) Khan SA; Kumar A; Varshney MK; Trikha V; Yadav CS: Dextrose prolotherapy for recalcitrant coccygodynia J Orthop Surg, Apr 2008, 16 (1) p27-9
8) Rabago D, Patterson J.Hypertonic Dextrose Injections (prolotherapy)for knee osteoarthritis: A Randomized Controlled Trial. Annals of Family Medicine May/June 2013 doi: 10.1370 vol.11 no.3 229-237
10) Reeves KD Hassanein K Long-term effects of dextrose prolotherapy for anterior cruciate ligament laxity: A prospective and consecutive patient study. Alt Ther Hlth Med May-Jun 2003, 9(3): p58-62.
11) Ryan M, Wong A, Taunton J. Favorable outcomes after sonographically guided intratendinous injection of hyperosmolar dextrose for chronic insertional and midportion achilles tendinosis. Am J Roentgenol. 2010 Apr;194(4):1047-53.
12) Topol GA, Reeves KD: Regenerative injection of elite athletes with career-altering chronic groin pain who fail conservative treatment: a consecutive case series. Am J Phys Med Rehabil 2008;87.
13) Yelland MJ, Glasziou PP, Bogduk N, et al. Prolotherapy Injections, Saline Injections, and Exercises for Chronic Low-Back Pain: A Randomized Trial. Spine 2004; 29(1): 9-16.)
Articles:
1) Cusi M, Sanders J. “The Use of Prolotherapy in the Sacroiliac Joint.” British Journal of Sports Medicine
2) Deganais S, Haldemean S, Wooley J. “Intraligamentous Injection of Sclerosing Solution (Prolotherapy) for Spinal Pain: a critical review of the literature.” Spine J 2005
3) Klein Robert G, Patterson Jeffrey. “Prolotherapy for the Treatment of Back Pain.” Position Statement of the American Association of Orthopedic Medicine
4) Rabago D, Slattengren A, Zgierska A. “Prolotherapy in Primary Care Practice.” Primary Care Clinics in Office Practice
5) Reeves K. Dean, Hassanein Khatab. “Randomized Prospective Placebo Controlled Double Blind Study of Dextrose Prolotherapy for Osteoarthritic Thumb and Finger Joints; Evidence of Clinical Efficacy.” Journal of Alternative and Complementary Medicine
6) Reeves KD, Hassanein K. “Randomized Prospective Double Blind Placebo Controlled study of dextrose prolotherapy for knee osteoarthritis with or without ACL laxity.” Alternative Therapy Health Medicine
7) Consensus Statement on the Use of Prolotherapy or Musculoskeletal Pain
The purpose of this paper is to explicate the theory, scientific evidence, methods, and applications for the procedure of Prolotherapy in the treatment of musculoskeletal pain. The example of knee osteoarthritis is used as an example as to why Prolotherapy should be used compared to other invasive therapies.
8) Tucker, Gloria – “Prolotherapy for Patients with musculoskeletal pain” – Marin Medicine Summer 2014
9) Local Frontiers – Pg 26-28